Articles
- Page Path
- HOME > J Mov Disord > Volume 2(1); 2009 > Article
-
Invited Review
Dopamine Agonist Therapy in Advanced Parkinson’s Disease - Heinz Reichmann
-
Journal of Movement Disorders 2009;2(1):10-13.
DOI: https://doi.org/10.14802/jmd.09003
Published online: April 30, 2009
Department of Neurology, University of Dresden, Dresden, Germany
- Corresponding author: Heinz Reichmann, MD, PhD, Department of Neurology, University of Dresden, Fetscherstraße 74, D-01307 Dresden, Germany, Tel +49-351/458-3565, Fax +49-351/458-4365, E-mail Heinz.Reichmann@uniklinikum-dresden.de
• Received: February 11, 2009 • Accepted: March 22, 2009
Copyright © 2009 The Korean Movement Disorder Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 36,301 Views
- 130 Download
- 3 Crossref
- “Parkinson’s disease (PD) doesn’t kill you, it takes your life away.” This is a disturbing quotation by the English Parkinson Lay Organisation. There is, however, no other neurodegenerative disease which responds better to treatment than PD. Treatment of advanced PD is located between these poles (Figure 1). Most national guidelines and papers on the treatment of PD recommended that early phases are treated with dopamine agonists and monoamineoxidase B inhibitors and late phases with levo-dopa. Common guidelines and publications regarding the treatment of late phase PD have thus not yet focused on dopamine agonists. This appears somewhat surprising because nowadays most patients commence treatment with a dopamine agonist. Strategic management of PD has to take into consideration the following points: 1) many patients will receive therapy for 15–20 years, 2) PD should be managed optimally throughout its course, 3) the aim of strategic management is to maintain efficacy and minimize side-effects in both the short and long term, and 4) initial therapy should be sustained for the long-term therapy. These criteria demand that treatment is initiated with efficacious and safe drugs and dopamine agonists meet this request.
- The main reason for their use is, however, that due to its short plasma half-life, levo-dopa induces dyskinesia. Conversely, dopamine agonists have longer half-lives and therefore stimulate dopamine receptors in a more tonic, continuous way, thus avoiding or at least decreasing the occurrence and severity of dyskinesia.1 It is for fear of the risk of developing side effects such as hallucinations, psychosis, orthostatic hypotension, nausea and vomiting that dopamine agonists are not normally used in advanced stages, rather than their loss of efficacy. For this reason, it would be most helpful to have measures to identify those patients with a high tolerance of dopamine agonists, in order to either allow them to continue with dopamine agonist therapy for as long as possible, or to add dopamine agonists in advanced stages.
- This review will briefly consider these options and will conclude that it may be beneficial to use modern dopamine agonists such as ropinirole slow release (Modutab™) or the rotigotine patch, even in the elderly or in advanced PD patients.
Introduction
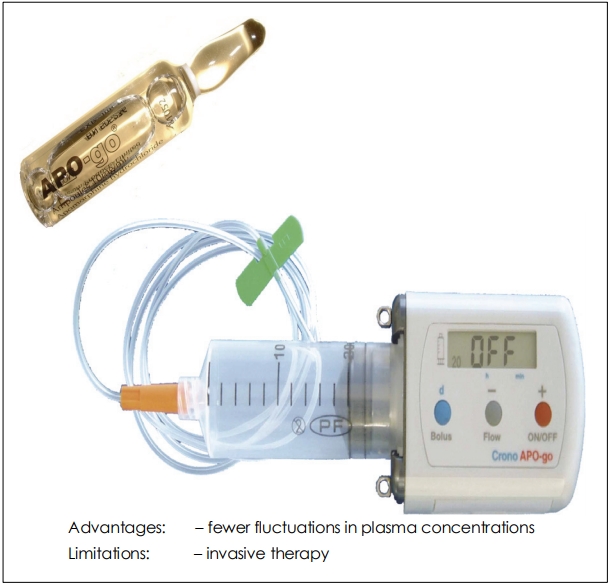
- Most patients with advanced PD receive levo-dopa or levo-dopa combined with a catechol-O-methyl transferase (COMT) inhibitor.2,3 Whilst this treatment reduces the risk of developing dyskinesia, it still does not appear to be as effective as a dopamine agonist with a long plasma half-life. Meanwhile, it has been shown that even taking multiple doses of a levo-dopa/COMT inhibitor preparation per day still results in peaks and troughs of levo-dopa blood levels and induces dyskinesia. Only the continuous supply of levo-dopa via the so-called “DuoDopa pump” is able to diminish the dyskinesia rate and to increase the number of “on” phases (Figure 2).4
- Analyses of the levo-dopa levels in the blood of such patients show a very constant concentration with less peaks and troughs, which is reflected by the low dyskinesia rate.5 This indicates that it is not the drug (levo-dopa) per se which causes dyskinesia, but rather its pharmacokinetics: when levo-dopa is supplied continuously, it is as good as dopamine agonists in preventing patients from becoming dyskinetic.
The Concept of Continuous Dopamine Replacement Therapy
- A perfect example of a pump therapy for PD is the apomorphine pump (Figure 3).6,7 Apomorphine has a plasma half-life of about twenty minutes, which is the shortest half-life of all dopamine agonists, however, if continuously delivered via a pumping system, apomrphine is highly potent in patients with advanced PD, and suppresses dyskinesia. Unfortunately, the subcutaneous application of the drug leads to serious skin irritation (panniculitis) in some patients, and some patients develop hallucinations, both serious side effects which lead to most patients stopping this treatment after two years. Thus, both the DuoDopa pump and the apomorphine pump are invasive methods which are associated with several problems.
- This is why deep brain stimulation is the most highly recommended and most often used therapy in the treatment of dyskinetic and advanced PD patients.8,9 Deep brain stimulation is achieved via electrodes which are inserted into both subthalamic nuclei. Most patients achieve a considerable improvement in mobility and a decrease in dyskinesia. Again, this is an invasive and risky method which also involves brain surgery. Thus, an oral medication which is as potent as these invasive measures and also safe would be desirable.
- It has already been outlined that dopamine agonists have a longer plasma half-life than levo-dopa. At the moment, cabergoline is the dopamine agonist with the longest plasma half-life (68 hours).10 Another important advantage of cabergoline is its once-a-day use, which results in very good compliance. In line with this, there are several reports which show that too high a fractionation of any medication, including anti-PD medication, leads to poor patient compliance.11 Unfortunately, due to the associated risk of heart valve fibrosis,12 cabergoline, together with pergolide, is now restricted to second line use. Aside from this serious drawback, cabergoline has proven to be associated with a low occurrence of dyskinesia and guarantees good mobility at night as well as during the day, which results in improved sleep. The first alternative to orally administered cabergoline was, at least in some countries, the dopamine agonist rotigotine, which is a non-ergot derivative and thus does not cause valvulopathy. Rotigotine is applied via a patch once daily (Figure 4). There are several convincing studies showing that the rotigotine patch not only guarantees continuous delivery of the drug, but is also highly efficacious.13 Side effects are similar to those found with oral non-ergot dopamine agonists such as ropinirole, pramipexole or piribendil. Rotigotine treatment resulted in statistically significant improvements in “off”-time, of responder rates, and an increase in “on”-time when compared to placebo in patients with advanced PD. In the so-called CLEOPATRA trial, non-inferiority to pramipexole was shown for reduction in “off”-time.14 Rotigotine was safe and well tolerated. Except for skin reaction at the site of application, the rate of adverse events was comparable for the pramipexole and rotigotine group.
- A new preparation of ropinirole was recently licensed. This slow-release preparation is administered in tablet form once daily, and plasma concentrations of the drug only decrease slightly over 24 hours. If ropinirole is taken in the morning, the plasma level of ropinirole decreases over night, which mimics the physiological situation in healthy persons: the ropinirole level in the blood in the morning is still high enough to guarantee a good start without early morning dystonia or akinesia.15 In the EASE-PD adjunct study, the efficacy and safety of ropinirole extended release (ER) was compared to placebo in advanced PD patients.16 Within two weeks there was a significant improvement in off-time with ropinirole ER. In addition, ADL scores improved as did nocturnal symptoms and mood. This is the first study in which the potential anti-depressive action of ropinirole was analysed. There was a significant improvement in the Beck Depression Inventory and quality of life also improved. This anti-depressive action may derive from the dopamine receptor D3-affinity of ropinirole.
- In all, several new studies are now available which confirm that dopamine agonists can be used even in advanced stages of PD. Motor symptoms (off and on time), dyskinesia rate, quality of life and mood were all improved. It appears from these studies that the continuous delivery of dopamine agonists prevents nausea, vomiting, somnolence or symptoms of a dopamine dysregulation syndrome. Typical symptoms of this latter syndrome are gambling, hypersexuality, binge eating or punding. It is speculated that the relatively constant medication levels in the blood and also supposedly at the dopamine receptors prevent the development of these side effects. In contrast, the plasma levels of ordinary dopamine agonists increase steeply shortly after intake, causing the above mentioned side effects. Thus, it is the new formulation of dopamine agonists which permits their use in advanced stages of PD. Within the next two years, an increasing number of long-acting dopamine agonists will become available. A lisuride patch and an ER formulation of pramipexole will both be available.
Dopamine Agonists in Advanced Parkinson’s Disease Patients
Figure 1.Limitations of multiple dosing for Parkinson’s disease. It is common practice to initiate dosing of L-dopa two or three times daily, however adjustments in dose level and dose frequency are often needed to maintain symptomatic control as the disease progresses. It is not uncommon for L-dopa to be dosed four or more times daily. Furthermore, frequent doses do not address the pulsatile delivery of L-dopa; there are still large fluctuations in plasma drug levels.
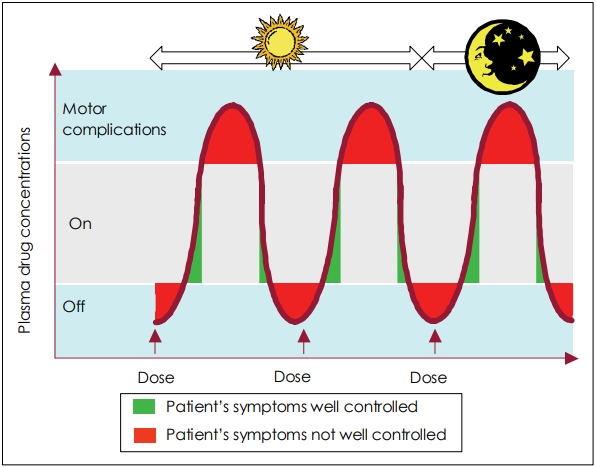
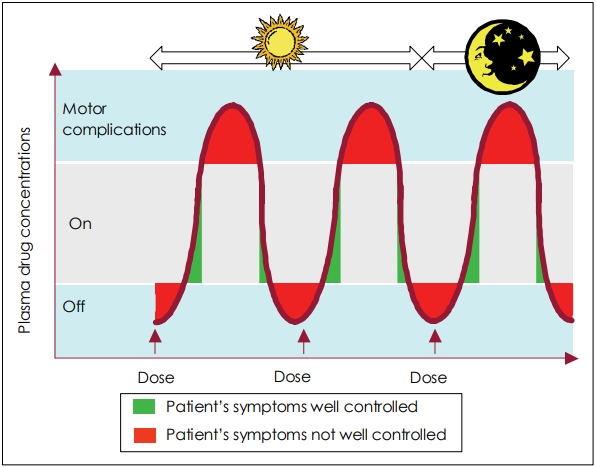
Figure 2.DuoDopa pump. DuoDopa is a combination of levo-dopa and carbidopa in the form of a gel that is administered directly into the small intestine through a surgically placed tube for advanced Parkinson’s disease. It can help maintain a constant plasma concentration of levodopa and reduce off time and incidence of dyskinesia.
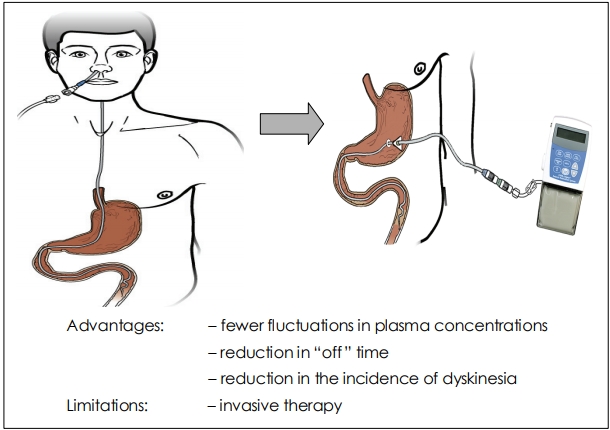
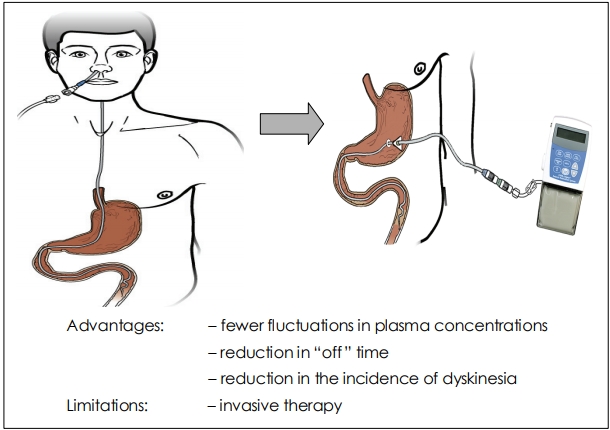
Figure 3.Apomorphine pump. Apomorphine is the shortest half-life of all dopamine agonists, however, if continuously delivered via a pumping system, apomrphine is highly potent in patients with advanced PD, and suppresses dyskinesia. PD: Parkinson’s disease.


Figure 4.Rotigotine patch. Control of motor fluctuations with ropinirole 24-hour prolonged-release. The ropinirole 24-hour prolonged-release improved awake ‘off’ time and this improvement was apparent at each clinic visit from week 2 to week 24. Furthermore, it was shown that ropinirole 24-hour prolonged-release was significantly more effective than placebo at all assessment time points in reducing awake ‘off’ time from 2 weeks onwards.16


- 1. Rascol O, Brooks DJ, Korczyn AD, De Deyn PP, Clarke CE, Lang AE. A five-year study of the incidence of dyskinesia in patients with early Parkinson’s disease who were treated with ropinirole or levodopa. 056 Study Group. N Engl J Med 2000;342:1481–1491.Article
- 2. Baas H, Beiske AG, Ghika J, Jackson M, Oertel W, Poewe W, et al. Catechol-O-methyltransferase inhibition with tolcapone reduces the “wearing off ” phenomenon and levodopa requirements in fluctuating parkinsonian patients. J Neurol Neurosurg Psychiatry 1997;63:421–428.ArticlePubMedPMC
- 3. Smith LA, Jackson MJ, Al-Barghouthy G, Rose S, Kuoppamaki M, Olanow W, et al. Multiple small doses of levodopa plus entacapone produce continuous dopaminergic stimulation and reduce dyskinesia induction in MPTP-treated drug-naive primates. Mov Disord 2005;20:306–314.ArticlePubMed
- 4. Nyholm D, Nilsson Remahl AI, Dizdar N, Constantinescu R, Holmberg B, Jansson R, et al. Duodenal levodopa infusion monotherapy vs oral polypharmacy in advanced Parkinson disease. Neurology 2005;64:216–223.ArticlePubMed
- 5. Stocchi F, Vacca L, Ruggieri S, Olanow CW. Intermittent vs continuous levodopa administration in patients with advanced Parkinson disease: a clinical and pharmcokinetic study. Arch Neurol 2005;62:905–910.ArticlePubMed
- 6. Colzi A, Turner K, Lees AJ. Continuous subcutaneous waking day apomorphine in the long term treatment of levodopa induced interdose dyskinesias in Parkinson’s disease. J Neurol Neurosurg Psychiatry 1998;64:573–576.ArticlePubMedPMC
- 7. Katzenschlager R, Hughes A, Evans A, Manson AJ, Hoffman M, Swinn L, et al. Continuous subcutaneous apomorphine therapy improves dyskinesias in Parkinson’s disease: a prospective study using single-dose challenges. Mov Disord 2005;20:151–157.ArticlePubMed
- 8. Deuschl G, Schade-Brittinger C, Krack P, Volkmann J, Schäfer H, Bötzel K, et al. A randomized trial of deep-brain stimulation for Parkinson’s disease. N Engl J Med 2006;355:896–908.ArticlePubMed
- 9. Kleiner-Fisman G, Herzog J, Fisman DN, Tamma F, Lyons KE, Pahwa R, et al. Subthalamic nucleus deep brain stimulation: summary and meta-analysis of outcomes. Mov Disord 2006;(Suppl 14):S290–304.ArticlePubMed
- 10. Rinne UK, Bracco F, Chouza C, Dupont E, Gershanik O, Marti Masso JF, et al. Early treatment of Parkinson’s disease with cabergoline delays the onset of motor complications. Results of a double-blind levodopa controlled trial. The pkds009 Study Group. Drugs 1998;55(Suppl 1):23–30.ArticlePubMed
- 11. Grosset D, Antonini A, Canesi M, Pezzoli G, Lees A, Swaw K, et al. Adherence to antiparkinson medication in a multicenter European study. Mov Disord 2009;Feb. 3. Article
- 12. Yamamoto M, Uesugi T, Nakayama T. Dopamine agonists and cardiac valvulopathy in Parkinson disease: a case-control study. Neurology 2006;67:1225–1229.ArticlePubMed
- 13. Watts RL, Jankovic J, Waters C, Rajput A, Boroojerdi B, Rao J. Randomized, blind, controlled trial of transdermal rotigotine in early Parkinson disease. Neurology 2007;68:272–276.ArticlePubMed
- 14. Poewe WH, Rascol O, Quinn N, Tolosa E, Oertel WH, Martignoni E, et al.; SP 515 Investigators. Efficacy of pramipexole and transdermal rotigotine in advanced Parkinson’s disease: a double-blind, double-dummy, randomised controlled trial. Lancet Neurol 2007;6:513–520.ArticlePubMed
- 15. Tompson DJ, Vearer D. Steady-state pharmacokinetic properties of a 24-hour prolonged-release formulation of ropinirole: results of two randomized studies in patients with Parkinson’s disease. Clin Ther 2007;29:2654–2666.ArticlePubMed
- 16. Pahwa R, Stacy MA, Factor SA, Lyons KE, Stocchi F, Hersh BP, et al.; EASE-PD Adjunct Study Investigators. Ropinirole 24-hour prolonged release: randomized, controlled study in advanced Parkinson disease. Neurology 2007;68:1108–1115.ArticlePubMed
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

- A Review of Advanced Molecular Engineering Approaches to Enhance the Thermostability of Enzyme Breakers: From Prospective of Upstream Oil and Gas Industry
Muhammad Naeem, Amjad Bajes Khalil, Zeeshan Tariq, Mohamed Mahmoud
International Journal of Molecular Sciences.2022; 23(3): 1597. CrossRef - ‘Dopamine agonist Phobia’ in Parkinson’s disease: when does it matter? Implications for non-motor symptoms and personalized medicine
Silvia Rota, Iro Boura, Lucia Batzu, Nataliya Titova, Peter Jenner, Cristian Falup-Pecurariu, K Ray Chaudhuri
Expert Review of Neurotherapeutics.2020; 20(9): 953. CrossRef - The Combination of DAT-SPECT, Structural and Diffusion MRI Predicts Clinical Progression in Parkinson’s Disease
Sara Lorio, Fabio Sambataro, Alessandro Bertolino, Bogdan Draganski, Juergen Dukart
Frontiers in Aging Neuroscience.2019;[Epub] CrossRef
Comments on this article
- Figure
- Related articles
-
- Fighting Against the Clock: Circadian Disruption and Parkinson’s Disease
- Apomorphine Monotherapy for Parkinson’s Disease: A Neglected Option?
- Gravitational syncope induced by rising elevators in a Parkinson’s disease patient
- Potential Link Between Cognition and Motor Reserve in Patients With Parkinson’s Disease
- Hand Movement-Induced Eyeblink Bursts in a Patient With Parkinson’s Disease
 KMDS
KMDS
 E-submission
E-submission
 PubReader
PubReader ePub Link
ePub Link Cite
Cite