Apathy and Olfactory Dysfunction in Early Parkinson’s Disease
Article information
Abstract
Objective
Olfactory and emotional dysfunctions are very common in patients with Parkinson’s disease (PD). Olfaction and emotions share common neuroanatomical substrates. Therefore, in this study, we evaluated the association between olfactory and emotional dysfunctions in patients with PD.
Methods
Parkinson’s disease patients who had been assessed for their olfactory function and neuropsychiatric symptoms including emotional dysfunction were included. A logistic regression analysis was performed to evaluate the association between low olfaction and different neuropsychiatric symptoms.
Results
The patients with low olfaction (cross cultural smell identification test score ≤ 6) showed a higher prevalence of apathy when compared with those with high olfaction, whereas the frequencies of other neuropsychiatric symptoms were comparable between the two groups. A multivariate logistic regression analysis revealed that the presence of apathy/indifference [odds ratio (OR) = 2.859, p = 0.007], age 70 years or more (OR = 2.281, p = 0.009), and the male gender (OR = 1.916, p = 0.030) were significantly associated with low olfaction.
Conclusions
Our results demonstrate that apathy/indifference is a unique emotional dysfunction associated with olfactory dysfunction in PD. The findings also suggest that PD patients with low olfaction have a high prevalence of apathy.
There is much evidence to support a close relationship between olfaction and emotion [1,2]. Certain odors reproducibly induce emotional states, and emotional induction modifies odor perception [2]. Olfaction and emotion share common neuroanatomical substrates, such as the amygdala, hippocampus, insula, anterior cingulate cortex, and orbitofrontal cortex [2]. Accordingly, dysosmia patients often experience depressive mood disorders and show a higher level of depressive tendencies when compared with normosmia controls [2–4].
Olfactory and emotional dysfunctions, such depression, anxiety and apathy, are very common in patients with Parkinson’s disease (PD) [5,6]. These dysfunctions often present in the premotor phase of PD [7]. Lewy bodies are found in the olfactory bulb and anterior olfactory nucleus in the PD brain [8]. The mechanism underlying emotional dysfunction in PD is unclear, although dysfunction of the mesocorticolimbic pathway and frontostriatal loop has been suggested [9].
Therefore, it is conceivable that olfactory and emotional dysfunctions are closely related in PD, i.e., patients with greater olfactory dysfunction may show greater emotional dysfunction. Only a few studies have investigated this relationship, and these have shown controversial results [10,11]. Cramer et al. [10] have found that olfactory impairment correlated with apathy in PD; however, Morley et al. [11] observed no significant association between olfaction and mood measures. Here we evaluated the association between olfactory dysfunction and emotional dysfunction in Korean patients with PD.
MATERIALS & METHODS
Subjects
Patients with PD who had undergone both the olfactory function test and neuropsychiatric symptom assessment during diagnostic work-up were selected, based on the medical records of the Yonsei Parkinson Center. PD was diagnosed according to the clinical criteria of the UK Brain Bank [12], and the patients showing subcortical ischemic change or infarction in basal ganglia on brain magnetic resonance imaging were excluded in this study. The informants for assessment of neuropsychiatric symptoms were limited to an actual caregiver. The patients who had an interval longer than 3 months between taking both tests were excluded. Because, in our hospital, olfactory function test was performed as a routine diagnostic work-up for PD, and neuropsychiatric symptom assessment was performed as a part of routine cognitive evaluation tests, we did not obtain informed consent for these tests. This study and the exemption of informed consent were approved by the Ethics committee of our hospital.
Assessment of olfactory function
The 12-item Cross-Cultural Smell Identification Test (CCSIT; Sensonics, Inc., Haddon Heights, NJ, USA) was used to assess olfactory function [13]. This test consists of a booklet containing micro-encapsulated odorants, which are released by scratching the bottom box with a pencil tip. The subjects were required to choose one of four alternatives.
Assessment of emotional dysfunction
The Korean version of the Neuropsychiatric Inventory (NPI) was used for assessment of emotional dysfunction [14]. For caregiver’s self-administration, a modified NPI worksheet was used [15]. Experienced neuropsychologists supervised the caregivers before administration, and checked that the worksheets were appropriate after administration. The caregiver who checked the patient’s neuropsychiatric symptoms was a patient’s family member, either a spouse or daughter and son, who was living together with the patient. The questions in each domain and scoring system were identical to the original version of NPI [16].
Statistical analysis
The distributions of each variable did not satisfy the assumption of normality in spite of a large sample size; therefore we used non-parametric analyses. To evaluate the relationship between CCSIT and demographic characteristics, we used the Mann-Whitney U test and Fisher’s exact test. The associations between the presence of each symptom of the NPI and CCSIT score were explored with Fisher’s exact test. Logistic regression analysis was used to adjust for potential compounders. The statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) version 20 (IBM SPSS, Armonk, NY, USA) and p-values less than 0.05 were considered to be significant.
RESULTS
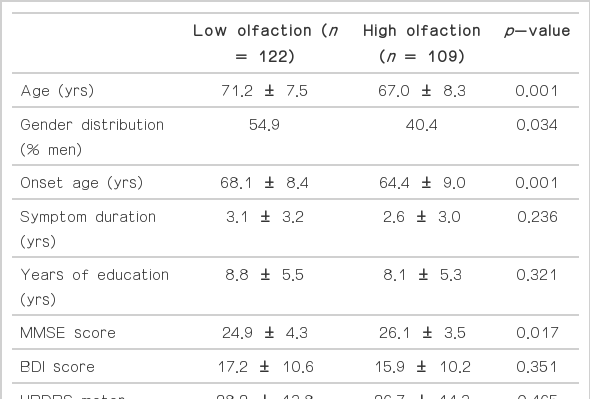
Two hundred and thirty-one patients (age, 69.2 ± 8.1 years; 111 men) were included in this study. According to the CCSIT score, we classified the patients into two groups: low olfaction (LO; CCSIT score of ≤ 6) and high olfaction (HO; CCSIT score of ≥ 7). One hundred and twenty-two patients belonged to the LO group, while 109 patients were in the HO group. The demographic data of the two groups are shown in Table 1. LO patients were older, experienced PD onset at an older age, and showed lower Mini-Mental State Examination (MMSE) scores than HO patients. The gender distribution was different in the two groups. Symptom duration, education level, Beck Depression Inventory score and Unified Parkinson’s Disease Rating Scale motor score were comparable between groups.
Neuropsychiatric assessments using the NPI are shown in Table 2. LO patients showed significantly a higher frequency of apathy when compared with HO patients (47.5% and 29.3%, respectively; p < 0.01), but the frequencies of other neuropsychiatric symptoms were comparable between groups. A multivariate logistic regression analysis was performed with degree of olfactory dysfunction as the dependent variable and age, gender distribution, MMSE score, and presence of neuropsychiatric symptoms included in the NPI as the independent variables. This analysis revealed that the presence of apathy/indifference [odds ratio (OR) = 2.859, 95% confidence interval (CI) = 1.337–6.114, p = 0.007), age 70 years or more (OR = 2.281, 95% CI = 1.233–4.217, p = 0.009), and the male gender (OR = 1.916, 95% CI = 1.065–3.447, p = 0.030) were significantly associated with the presence of LO (Table 3).
DISCUSSION
This study showed that the presence of apathy/indifference was significantly associated with low olfactory function in PD patients. The presence of depression/dysphoria or anxiety was not related with the degree of olfactory function. In addition to the emotional dysfunction evaluated in this study, age as well as older age at PD onset, and the male gender was also associated with low olfactory function. The association of low olfaction with old age and male gender is well-recognized in PD patients as well as in the general populations [17,18]. The present results suggest that PD patients with low olfaction have a high prevalence of apathy.
Cramer et al. [10] performed an apathy evaluation scale and CCSIT in 70 patients with PD and found that patients with a higher apathy scale (i.e., apathetic PD) showed a lower CCSIT score when compared with patients with a lower apathy scale (i.e., non-apathetic PD). In addition, they also observed that apathetic patients showed a higher depression score when compared with non-apathetic patients, but found no correlation between CCSIT score and depression score [10]. Although they did not measure any other neuropsychiatric symptoms, their results are somewhat compatible with the present results. In contrast, Morley et al. [11] performed various neuropsychiatric assessments including depression, anxiety and apathy scales, and cognitive tests in 248 PD patients, and demonstrated that there was no significant association between olfaction and mood measures. However, psychotic symptoms and poor cognitive function such as memory and executive function were associated with low olfaction [11]. Currently, we are unsure of the reason for the discrepancy between Morley et al. [11] and those of the present study, in addition to the results of Cramer et al. [10] However, it may be related to different subject populations; in this study, patients are at an earlier stage of PD and a higher proportion of female. We also use different methods for assessing emotional and olfactory dysfunction.
Odors elicit emotion and are linked to emotional memory [1]. Different odors can elicit individual affective responses which may be pleasant or unpleasant [1]. Olfactory dysfunction in PD develops several years or even decades before motor symptoms [19,20]. Reduced olfactory stimulation for a long-period might reduce emotional memory as well as emotional responses to the external environment, resulting in apathy/indifference to external stimuli. Human neuroimaging studies have demonstrated that the amygdala and orbitofrontal cortex are activated by unpleasant or pleasant odors, consistent with their function in emotion [21,22]. In addition, hypometabolism in the anterior cingulate and orbitofrontal cortex are associated with apathy in Alzheimer’s disease [23,24]. These reports provide evidence to support the relationship between a loss of olfactory function and reduced emotional response. Although depression was often reported to be correlated to apathy [10,25,26], it seems unrelated to olfactory dysfunction in PD in the present study, similar to the previous study [11].
The MMSE score was lower in patients with low olfaction, however logistic regression analysis revealed that it was not associated with low olfaction. This result is agreement with that of Morley et al. [11] However, in their result, low olfaction was associated with the performance in Tower of London test or verbal memory task [11]. On the other hand, several studies showed that apathy was related with cognitive impairment [25], especially frontal/executive dysfunction [27]. Taken together, frontal/executive dysfunction might be a possible link between olfactory dysfunction and apathy, but further investigations are required to clear this association.
Our study has a number of limitations, such as a retrospective inclusion of patients and no quantification of emotional symptom severity due to the narrow range of each symptom scale in the NPI. The NPI was originally designed for assessing psychiatric symptom mainly in patients with Alzheimer’s disease [16], and hence, it may not be suitable for PD. Olfactory dysfunction is usually non-progressive once motor symptoms develop, while apathy can be progressive throughout the course of PD [10]. Thus, a prospective and longitudinal follow-up study is required in the future to evaluate changes in the degree of apathy relating to olfactory dysfunction in PD.
Notes
Conflicts of Interest
The authors have no financial conflicts of interest.